
What is Cervical Radiculopathy or Nerve Pinched in Neck and How to Treat it?
What is Cervical Radiculopathy?
The neck is made up of 7 bones called the cervical vertebrae. These vertebrae are not uniform and in fact change structure depending on the level. For instance, the top two vertebrae, C1 and C2, are called Atlas and Axis.
C1, Atlas, has a structure which connects to and holds the skull on to the spine. This description is much like the titan god Atlas, who was said to have held the weight of the heavens on his shoulders as a punishment. C1’s structure means that it is firm and secure but movement is confined.
C2, Axis, bears its name from the pointed structure that fits perfectly into its neighbour, C1. This pointed design allows C1 to rotate around C2’s axis.
However, increased mobility affects C2’s structural stability.
From the first two vertebrae we begin to realise how much structure affects the vertebrae’s function.
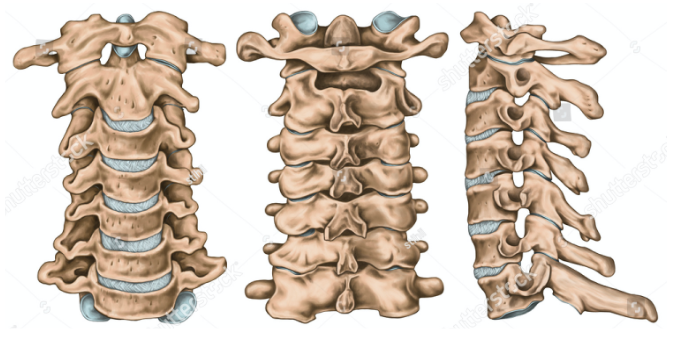
In contrast to the initial two vertebrae, the next five are relatively similar, the greatest change being the ‘spinous processes’ or bony struts that protrude backwards (seen clearly in a side profile in the furthest right picture above). As the vertebrae progress down from C3-C7, the spinous processes become more flattened and increase in length. Similar to spinous processes, the transverse processes become larger and protrude further out of each side of the vertebrae. Both processes act as attachment points for muscle and connective tissue.
The cylindrical vertebral bodies seen in a front-on position in picture one and a side profile on picture three are separated by flexible fluid filled pads called a vertebral disk. These act as shock distributors, displacing the forces sent through the neck and spine.
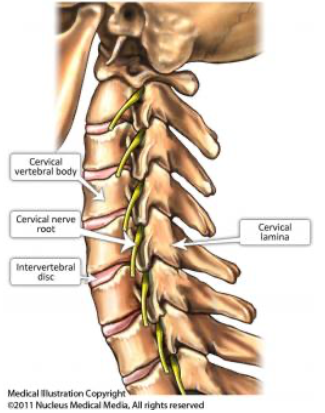 In the space inside the Y-shaped structure of the spinous process and the circular vertebral body, the spinal cord is found. This runs through the length of the vertebral column and serves as a main hub for nervous tissue, called the central nervous system (CNS).
In the space inside the Y-shaped structure of the spinous process and the circular vertebral body, the spinal cord is found. This runs through the length of the vertebral column and serves as a main hub for nervous tissue, called the central nervous system (CNS).
Nervous tissue is not confined to the CNS and in fact spans from here into all the tissues of our bodies via nerve pathways, in some movement is performed and in many more, sensation, temperature and proprioception is felt. These nerve pathways start with nerve roots that pass out of the CNS, via small spaces in between the vertebrae. When these nerve roots become irritated, compressed or damaged the person may feel symptoms localised to that area. However, what is more likely is that they may travel down the related nerve pathway. This is called cervical (neck) radiculopathy (radiating pain).
Cervical radiculopathy is therefore an umbrella term that can be used to describe the symptoms that you may feel as a result of conditions such as disk herniation, spinal stenosis and other spondylopathies. With this in mind, lots of people have been shown to display common age related degenerative conditions such as these, and not experience any symptoms at all. Therefore, structural changes are not always related to painful experiences and vice versa.
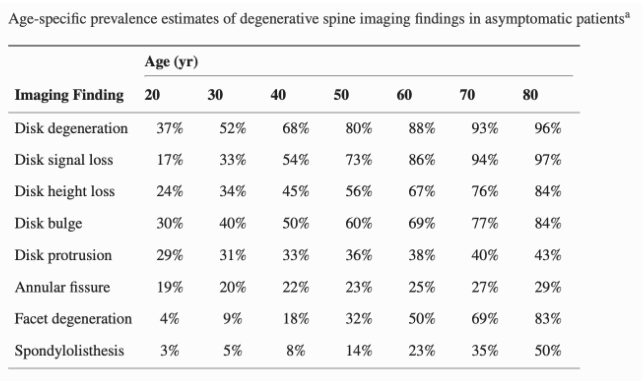
For instance, this study by Brinjikji, W. et al. (2015) used MRI/CT imaging to screen healthy individuals with no pain symptomatology. Their results showed that much of this population displayed evidence of age related changes, such as disk degeneration and bulge, with no pain. Highlighting the fact that these changes are normal for ageing populations. In some cases people experience a painful response and in others, they do not.
How Common are Cervical Radiculopathies?
- Cervical issues are one of the most common conditions that physiotherapists and doctors will see.
- Around ¼ of the global population will have a neck issue once in the year.
- Around ½ of the global population will suffer from a severe neck related issue once in their lives.
- Increased likelihood in ages 40-49.
What are the Common Signs and Symptoms?
The following symptoms may be present at the neck and upper limbs:
- Pain
- Changes in sensation
- numbness, tingling, pins and needles sensation
- Reduced available movement
- Reduced ability
Differential Diagnoses
Below are a few examples of diagnoses that appear similar to cervical radiculopathy.
- Shoulder Pathologies – many shoulder conditions can cause symptoms that are interchangeable with cervical radiculopathies.
- Spinal Tumour – Tumours are less common, but may display similar symptoms.
- Cervical Muscle Conditions – muscle injuries can cause pain, weakness and restricted ROM, mimicking cervical radiculopathies in some cases.
- Peripheral Nerve Disorders – conditions that affect the nerve tissue outside the spine and brain are called peripheral neuropathies. The symptoms experienced for irritation to the cervical nerve roots in a cervical radiculopathy is very similar to that of a peripheral neuropathy affecting the neck and arm.
- Thoracic Outlet Syndrome – this rare disorder affects the blood vessels that travel between the collarbone and ribs. When this occurs, symptoms can include tingling/numbness in the arm and fingers, and pain in the neck and surrounding areas.
What Makes it Worse?
- compression of the cervical spine (extension/side flexion) on the problem side
- Rotation towards the problematic side
| Case Study:
A patient enters the clinic with a shoulder complaint. He is experiencing pain at his right shoulder, travelling down into his arm. His middle, index and thumb fingers are numb and tingly and he’s struggling with rotating his head to the right. When asked about the onset he cannot think of a definite cause. However, he does recall that the symptoms have increased as work has become especially stressful. What tests should be used to further our investigation? |
Assessments/Tests
What do people tell us? (Subjective)
- Pain will often be felt localised in a region of the neck
- Patients may also describe pain at the shoulder, upper back region and upper limb.
- This pain may be accompanied with neurological changes in sensation (such as tingling, pins and needles, numbness and inability to distinguish between textures).
- It may be accompanied with changes in functional ability, such as reduced strength, reduced movement available, less controlled or clumsy movement and increase in pain levels on movement.
- They may tell us that specific movements promote pain and worsen the symptoms.
- Symptoms may have been caused by a specific event
- Symptoms may have built up over a period of time
What do we find on physical assessment/testing? (Objective)
Visual
The person may be holding the neck in a slightly tilted, pressure relieving position. This may be conscious or they may be totally unaware.
Palpation
(Touch and Feel)
Pain may be provoked when pressing on and around the area.
The muscles of the neck may be tight and stiff.
Range of Motion (degree of movement)
Neck and upper limb movement may be decreased, this may be limited by strength and also may be due to pain.
Special Tests
- Spurling’s Test – where the head is tilted into lateral flexion, and the assessor provides over pressure of approx 7kg.
- Upper Limb Nerve Tension-1 – Neurodynamic mobilisation, primarily assessing the median nerve. Bring shoulder into abduction and external rot., arm extension, forearm supination, wrist extension.
- Distraction test – traction forces applied to the neck, by grasping the mastoid process and pulling away from the body. Test is positive if symptoms alleviate with traction forces.
- Involved side neck rotation range of motion less than 60 degrees.
When all 4 of these clinical features are present, the post test probability of cervical radiculopathy is 90%, Where only 3 of the 4 tests are positive the probability decreases to 65%.
Investigations/Scans
As discussed previously, imaging may provide insight into the problem at hand. However, there are complexities that we must be aware of when considering imaging. Such as normal, age related changes that are often asymptomatic. In addition to this, imaging results may in fact influence our pain negatively.
CT Scans
Both CT and MRI have been used to assess cervical radiculopathy; however, neither is required for diagnosis of cervical radiculopathy and neither is indicated unless patients have failed a (6-week) course of conservative therapy. CT scanning cannot accurately demonstrate the commonest cause for cervical radiculopathy (disc herniation) without myelography, which requires hospital admission, lumbar puncture and the use of contrast. The assessment of root compression of the cervical spine by CT scan has fair-to-moderate reliability.
Magnetic Resonance Imaging (MRI)
In patients with cervical radiculopathy, MRI is the imaging technique of choice for the detection of root compression by disc herniation and osteophytes. MRI allows the nerve roots to be directly visualised. However, imaging studies often report findings that may have little to do with neck pain and there may be a high prevalence of incidental neck abnormalities with MRI. Incidental findings would be expected to increase with age.
X-Ray
X-ray imaging would be able to illustrate boney changes that may have occurred at the spine.
Treatments
Conservative Treatment
Physiotherapy
| Passive rehab | Active rehab |
| PEACE Protocols
Protect – Protect from further injury Elevate – avoid pooling Avoid NSAIDS – allow inflam. cycle Compress – reduction of inter Education – avoid catastrophizing/fear |
LOVE Protocols
Load Optimally – load that structure! Optimism – Be positive, it will heal. Vascularisation – early mobilisation and increased Exercise – get back into pain free movement! |
| Manual therapy – Mobilisation and manipulation movements can be used to aid in pain relief and range of motion in the short term. | Mobility training – As a general rule, stretches should be participated in a position to mitigate pain response, light discomfort is fine, pain is not the aim. |
| Acupuncture – Localised microtrauma, increases blood flow to the local area.
Pain experience modulation Neurotags |
Strength training – Strength training should be focussed on the neck, upper back, and surrounding shoulder blade muscles. |
| Bracing – soft braces can be used to reduce load on the neck joints. However, use should be restricted as >2 weeks is related to muscle wastage. |
Some additional treatments that a physio may offer you:
- Taping for support and pain relief
- Advice on supplements for pain reduction and injury recovery
- Possible work station assessment/postural assessment
- Specialist equipment, such as bracing, and rehabilitation equipment
Home exercises that may help – V = check out our YouTube for example videos!
Stretching
- Chin Tucks V
- ULNT1 V
- Cat/Camels V
- ULNT’s – depending on the presentation
- Cat camel 1
- Eagle
- Pec stretch
- Bow/arrow
- Mermaid
- Single arm rolls
- Cervical Lateral flexion L/R
- Levator scapulae stretch
- suboccipital extension
Strengthening
- Supine chin tucks and cervical flexion
- Shoulder retractions with res. band
- Y raises
Some advance exercises that you may try as you become stronger
1) C spine – chin tucks with rot, Cat/camel with chin tuck
2) shoulder/scapulo-thoracic – mermaid, open book
3) Pilates specific –
Matt work: Thread the needle
Trapezius: Neural slides, Arm bar scapula slides/Extension,
Multichair: Prone extension, Single arm Rotation,
Reformer: Supine arm work, Prone ext/Scap slides
| SIDE NOTE: Exercises performed in seated should be done so in a maximally upright posture, slouching will cause the neck to extend (tilt backwards) and restrict movement at the facet joints. |
Non-conservative Treatment
Injection therapy
Epidural steroid injections are a common treatment modality for cervical radiculopathies. Guided by dye and medical imaging, a surgeon will guide an injection into the epidural space, depositing anti-inflammatory steroids that may benefit in regard to the patients pain levels.
There are mixed results regarding the outcome of this treatment, and each person’s case must be scrutinised before agreement is made to refer for surgical input such as this. Risks apply and must be weighed up against the potential gains.
Surgery
There are multiple forms of surgeries to target cervical radiculopathies. This is due to the variety of conditions that can result in the neck pain symptomatology. These procedures include decompression surgeries, decompression followed by fusion of the vertebrae, removal of parts of the vertebrae called the laminae and also surgeries that widen aspects of the foramina, where the nerve itself passes out of the vertebrae.
Just like injection therapy, surgery has a risk attached to it and therefore conservative treatment is the first port of call. If this is not effective in the first 6 weeks then surgery will be considered. Even then, factors such as age, BMI and other health factors will influence the likelihood of the patient being elected for the procedure.
Prehab
Surgery should be preceded by a well structured prehabilitation programme to prime the area and optimise recovery rate following surgery.
This should involve strengthening the surrounding muscles, working on flexibility and mobility at/control of the vertebral segments. In addition to this, general strength training and cardiovascular exercise will be beneficial for the outcome of the surgery.
Post Surgery
Following on from surgery, post-operative management will involve a specific exercise programme. This is generally guided by a multidisciplinary team consisting of the orthopaedic surgeon and the physiotherapist.
Due to the nature of the variety of surgeries available, specifics for the post operative intervention cannot be given.
However, you can expect to follow a period of immobilisation and restricted load and range management. This is generally followed by a period of increased movement through the joints (range of motion), followed by light weight and high repetition movements, lastly finishing with increased resistance, lower repetitions.
Progression through this post-op programme and specific exercise prescription will be specified to the surgery, the surgeon and physio’s preference and patients ability.
Key take-home messages
- Cervical neuropathy is an umbrella term used to describe the symptoms of various neck related disorders such as disk bulges and stenopathies. It is a common musculoskeletal disorder that is often experienced as pain in the neck that travels down into the shoulder and upper limb.
- Cervical neuropathies can be confirmed to a 90% accuracy with the use of four tests. They include the Spurling’s Test, Upper Limb Nerve Tension-1, Distraction test and neck rotation test. If ¾ are apparent, then the prognosis becomes only 65% accurate.
- Treatment for cervical radiculopathy includes a variety of passive and active modalities. These include the use of passive treatments such as manual therapy, bracing and acupuncture. However, an active approach to stretching, mobilisation and strengthening of the neck and surrounding musculature is necessary for long standing relief.
- Lastly, surgery should be considered if conservative treatment is not successful at 6 weeks, or if symptoms progress in this time.
References:
Brinjikji, W., Luetmer, P. H., Comstock, B., Bresnahan, B. W., Chen, L. E., Deyo, R. A., Halabi, S., Turner, J. A., Avins, A. L., James, K., Wald, J. T., Kallmes, D. F., & Jarvik, J. G. (2015). Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR. American journal of neuroradiology, 36(4), 811–816. https://doi.org/10.3174/ajnr.A4173




