
What is Ankle Inversion Sprain and How a Physio can help?
What is an Inversion Sprain? 
The ankle joint is made up of the following three bones.
- The Tibia is the main shin bone, running from your knee to your foot
- The Fibula is the smaller of the two lower leg bones
- The Talus is a foot bone that fits into the shape created by both the tibia and fibula forming the lower portion.
The ankle joint is a hinge joint, meaning it allows hinge-like movements, such as pointing the foot down (plantarflexion) and raising the foot up (dorsiflexion). Its bracket shaped structure means that all other movements are restricted, such as tilting the foot to the outside and inside and rotating is not possible. In addition to this the talus is wider at the front and thinner at the back, making the foot weaker and less stable in a plantarflexed position, when the talus is at its thinnest.
The muscles around the ankle include, but are not restricted to:
- The gastrocnemius and soleus (calf muscles),
- The Tibialis anterior (the shin muscle)
- The peroneal muscles (outer-leg muscles) and posterior tibialis (inner-leg muscle).
Holding the lower leg bones to the foot are a series of ligaments, half of which cover the inner side of the ankle, called the medial/deltoid ligaments, they include the posterior tibiotalar ligament, tibiocalcaneal ligament, tibionavicular ligament and the anterior tibiotalar ligament.
The other half covers the outer side, the lateral ligaments, they include the anterior talofibular ligament, calcaneo-fibular ligament and posterior talofibular ligament. The role of these ligaments is to restrict excessive movements of the foot, especially through inversion and eversion.
When these ligaments are over stressed, often by forced inversion, or less commonly, forced eversion, the tissue can become damaged, resulting in a ligament sprain.
Who Gets Inversion Sprains?
An inversion sprain will generally be caused by one of two factors:
- The sprain may be caused by a high-impact injury. In which someone may describe:
“I was playing football and as I jumped to catch the ball I lost my balance slightly and landed funny on my foot. My ankle became very painful, hot and swollen.”
OR
- the sprain may be due to weakness or deconditioning of the ankle. Where someone may describe:
“I was walking the other day and out of nowhere rolled my ankle. It’s really painful, but I’m pretty used to it. It’s happened a few times now over the years.”
Common Risks Factors for Inversion Sprains:
- Perhaps the most frequently studied risk factor for lateral ankle-ligament sprains is a previous sprain of this complex.
- Tyler et al. (2006) noted that BMI was a significant risk factor for ankle sprain in high school American football players. They reported ankle-sprain IRs (per 1000 exposures) of 0.52 for players with a normal BMI, 1.05 for players at risk of being overweight, and 2.03 for overweight players.
- Watson et al. (1999) found that male soccer athletes who sustained ankle sprains had greater height than those who did not. Milgrom et al. (1991) reported that during basic training, male military recruits who were taller and heavier were at increased risk of suffering an ankle injury.
- Roos et al. (2016) determined LAS was the most common injury diagnosis in 12 sports and in the top 5 for an additional 9 sports. The sports with the highest rates of LAS were men’s basketball.How Common are Inversion Sprains?
Inversion sprains are common, especially in younger populations. One study completed in the UK looked at data from four geographical districts and found that:
“The female population most commonly affected was 10-14 (12.8 per 1000). Additionally, males, aged 15-19 were most frequently affected 12.0 per 1000)”
However, the risk of inversion sprain increases dramatically in populations such as those who participate in sport, or have a high intensity occupation, such as within the armed forces.
Assessments/Tests
What are the Common Signs and Symptoms?
- Reduced movement available, especially into Eversion/inversion.
- The ankle and foot may be swollen and bruised
- Your injury will likely have been part of a memorable event (e.g. twisting your ankle when landing from a jump)
- Pain at the ankle and foot, especially under the bony prominence on the outside of the foot
- Pain on palpation of the outer aspect of the foot and ankle joint
Differential Diagnoses
- Syndesmosis
- Tarsal Tunnel Syndrome
- Cartilage or osteochondral injuries
- Peroneal Tendinopathy or subluxation
- Posterior Tibial Tendon Dysfunction
What Makes it Worse?
- Pain may increase on standing, walking or weight-bearing through the foot
- Palpation (pressing) on the ligament and surrounding structures
- Symptoms can often worsen at night or first thing in the morning, but may relieve after a short while
- Movement at the foot and ankle
What do We Find on Physical Assessment/Testing? (Objective)
-
- Visual – visually, the foot may appear swollen, bruised or red,
- Palpation – the area may feel hot to the touch. It will likely be painful on palpation.
- Range of Motion – Range of motion will likely be painful in most directions, especially down and inwards.
- Strength – reduction in calf or peroneal strength, possibly due to pain or chronic re-injury
Special Tests
- Anterior Draw – tests the ATFL
- Talar Tilt – tests the CFL
- Posterior Draw – tests the PTFL
- Squeeze test – for syndesmotic sprain
- External rotation stress test (Kleiger’s test) – syndesmotic sprain
It is recommended that these tests be performed at 4-7 days post acute injury to allow the initial swelling and pain to settle, enabling the therapist to gain a more accurate diagnosis.
Scans: X-Ray
As a general notion, the Ottawa rule should be used to determine the need for food radiography.
Component to Test:
- Bony tenderness along distal 6 cm of posterior edge of fibula or tip of lateral malleolus
- Bony tenderness along distal 6 cm of posterior edge of tibia/tip of medial malleolus
- Bony tenderness at the base of 5th metatarsal
- Bony tenderness at the navicular
- Inability to bear weight both immediately after injury and for 4 steps during initial evaluation
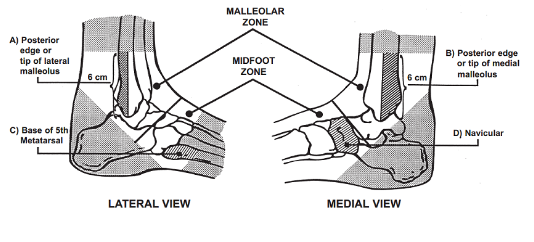
An Ankle X-ray is only required if:
- There is any pain in the malleolar zone; and,
- Any one of the following:
- Bone tenderness along the distal 6 cm of the posterior edge of the tibia or tip of the medial malleolus, OR
- Bone tenderness along the distal 6 cm of the posterior edge of the fibula or tip of the lateral malleolus, OR
- An inability to bear weight both immediately and in the emergency department for four steps.
A foot X-ray series is indicated if:
- There is any pain in the midfoot zone; and,
- Any one of the following:
- Bone tenderness at the base of the fifth metatarsal (for foot injuries), OR
- Bone tenderness at the navicular bone (for foot injuries), OR
- An inability to bear weight both immediately and in the emergency department for four steps
Treatments
Conservative Treatment
Physiotherapy treatments that a physio may offer you:
Advice regarding PEACE/LOVE protocols
A physiotherapist is educated on the principles that surround the peace and love protocols and are therefore in a position to pass this knowledge onto patients in a way that they can understand.
In the acute stages of injury the following actions are recommended:
- Protection
- Elevation
- Avoiding anti-inflammatory drugs (not applicable in some situations)
- Compression
- Education
Followed by the following in the more chronic stages:
- Loading Optimally
- Optimism
- Vascularisation
- Exercise
This evidence based protocol was developed by Blaise Dubois and Jean-Francois Esculier for the BJSM in 2019, as a tool to follow on from acronyms such as RICE, PRICE or POLICE.
Manual therapy
Mobilisation and manipulation movements can be used when the inflammatory stage has subsided, to aid in pain relief and range of motion in the short term. NICE guidelines recommend the consideration of manual therapy (spinal manipulation, mobilisation or soft tissue techniques such as massage) but only as part of a treatment package including exercise.
Acupuncture
Practitioners such as Geoff Maitland and Ronald Melzack have long practised the notion of counterirritation and localised microtrauma. Acupuncture is one form of this methodology that aims to increase activity and blood flow to the local area, promoting healing. The theory behind it is multifactorial, one of which proposes that localised noxious stimulation at the injury site activates the descending inhibitory systems, reducing nociceptive transmission to the brain from the level of the spinal cord, relieving pain. This process is mediated by the enkephalin group of endogenous opiates, released at spinal and supraspinal levels (Fields et al 2006).
Strapping, Taping and Bracing
Strapping, taping and bracing are all forms of external support that can be used to protect the area, aid in movement, and act as a sensory reminder of the injured structure whilst the area recovers. It is well known that strapping, taping and bracing can be used as a valuable adjunct tool in the physiotherapists arsenal, especially in the acute stages of an injury. However, such intervention should not be considered as a sole treatment option (Nelson NL et al., 2016).
Advice on anti-inflammatory agents and creams
Although PEACE/LOVE protocols advise against the use of anti-inflammatory agents in the acute phase of injury, in some cases, the need for a reduction of inflammation is great. The medium in which anti-inflammatory aids can vary depending on the nature of the inflammation and therefore advice on which to use may vary from person to person. This may include topical creams, oral tablets or even supplements rich in natural anti-inflammatories such as curcumin, often ingested for anti-inflammatory effects at a dose of about 5 g/day.
Advice on supplements for injury recovery
In addition to this, advice may be provided on nutrient intake, such as the increased demand for protein, up to 2.2g/kg (that’s a lot!) when injured, or the benefits of creatine monohydrate supplementation, for lean muscle mass and strength retention during periods of forced inactivity. Both have been researched heavily, both display excellent safety profiles (Rawson, E. S. et al., 2018).
Equip you with specialist equipment, such as foam rollers, bands, etc.
In addition to educating and prescribing a treatment approach, a physio is able to equip the individual with all the necessary equipment for their rehab journey. This may include resistance equipment, orthotics, braces, mats or mobility aids, making the process fluid and simple.
Home exercises that may help – V = check out our YouTube for example videos!
Stretching
- Alphabet ankle rolls
- Good toes and naughty toes
- Active lifting of inside and outside foot (inversion/eversion)
Strengthening
- Dorsiflexion with resistance
- Plantar flexion with resistance
- Stable base – single leg stands
Exercises you may progress towards as you become stronger:
1) Unstable base – Stands/single-leg stands/squats
2) Strength – Peroneal/gastroc/soleus muscle work
3) Low-intensity force – calf pulses, toe walking
4) Dynamics – Single leg hops, zig-zags, skipping,
5) Pilates Specific –
Matt work: dowards dog, TA stretch (doub/sing leg)
Trapeze: roll down/unstable base, thigh stretch?
Multi-chair: Step up series,
Reformer: russian splits, side lying: single leg press (strap)
Key Take-home Messages
- LAS is generally caused by rolling the ankle inwards/awkward landing and can cause sudden sharp pain at the outer ankle region.
- Younger individuals participating in sports such as basketball and soccer are most likely to experience LAS due to the physical demands.
- Initially after injury → 3-4 days, pain may increase on standing, walking or weight-bearing through the foot
- Scans can be used if there is any obvious bony abnormality or if sharp pain (which limits walking) persists for >4-5 days
- Conservative physiotherapy treatment including joint mobilisation, taping and progressive strengthening can reduce symptoms and address the root cause of the issue.




