Reading X-Rays, CT & MRI Scans: What Does It All Mean?
How often have you had an X-Ray, CT or MRI scan done and read the report only to realise that none of it makes sense? This often happens when people come in to see us with their scans. Some practitioners and GP’s are really good at taking the time to translate the findings, but often they just seem to be written in a complete other language! This always seems particularly frustrating for people, who are usually in pain, and just want to find out what the cause of that pain is.
What are the different scans looking at?
Before we start explaining what the scans may find, I feel it is important to clarify why there are different scans and what each one is basically looking at (at a musculoskeletal level).
X-Rays look at the hard structures; the bones. As the X-rays don’t travel as well through bone (the bones absorb them), the bones will appear white – while the other structures, such as muscles, organs and fat, will appear darker/black because they allow the X-rays to pass through them. X-rays can also be used to give an idea of the amount of joint space (eg. In the knee), but they cannot clearly see the joint structures (including cartilage, ligaments) or muscles. They can give an idea of “wear-and-tear” around a certain area, and can be used to diagnose arthritic changes.
CT (Computed Tomography – also known as CAT) scans use X-Rays and then digital computer technology to create the images from the X-ray pictures. They will look at bones, joints, blood vessels, nerves and soft tissues – but this may give a less clear image compared to that from an MRI (although an MRI is often not needed).
MRI (Magnetic Resonance Imaging) scans are usually considered the “gold standard” in scans, as they will usually show up everything (providing there’s something to find). They will look at bones, joints, blood vessels, neural structures, muscles, and tendons. They use strong magnetic fields and radio frequency pulses to create the 3D image of the body part being scanned. This is usually considered the clearest image out of all the options.
Why are they helpful?
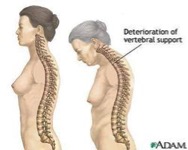
Scans can be a great way to visualise what is happening inside, in order to provide a clearer diagnosis. It is an important point though, that the findings on the different types of scans are not necessarily correlated with pain. For example, people who may not be in pain can have terrible-looking scans. While others that are in pain may wonder why nothing has turned up on their scan. This can be really frustrating, and leave someone to wonder what is actually happening to cause their pain – and why it hasn’t shown up. For this situation, it is important to realise that there are certain things that will not show up on any scans. These can include, but are not limited to, muscular tightness (scans will show tears, but not tightness), joint stiffness, muscle imbalances, postural changes, and general functional issues (they will show up structural problems only). These can lead to painful problems, but will not turn up on the scans – although your physiotherapist will certainly be able to feel them! (This is why it is a good idea to follow up with your physiotherapist, even if your scan comes back “normal”).
So, what does it all mean?
There are certain ‘foreign’ medical terms that turn up on the different scans, and I’ll go through them now. I’ll separate them into common musculoskeletal terms found on X-Ray, CT and MRI scans. The terms below will mainly relate to lower back scans (unless otherwise indicated), as they can be the most confusing!
X-Ray findings
Bony osteophytes – bony growths around the joint line, usually a sign of degeneration (AKA. Bone spurs)
Degenerative changes – signs of “wear & tear” around the joint, which can include reduced amount of cartilage, loss of joint space, and signs of bony osteophytes.
Loss of joint height (esp. with the knee) – a sign of “wear & tear”, indicated on X-Ray by a reduced gap between the bones (especially with a weight-bearing radiograph)
CT scan findings
Central canal stenosis – Narrowing (stenosis) of the main canal that the spinal cord sits in. This is a degenerative condition, usually associated with a degenerative disc bulge (see description below in MRI)
Facet arthropathy – degeneration of the facet joints (may be a sign of osteoarthritis)
Neural foraminal narrowing/stenosis (or exit foraminal stenosis) – Narrowing of the space where the nerve exits the spinal column. This can cause pressure on the exiting nerve root, and can often be caused by a disc bulge, osteophyte growth or collapsed disc space.
Posterior disc bulge – A bulge in the vertebral disc in the backward (posterior) direction. This can also be noted as “Posterolateral disc bulge” if the bulge goes backwards and also off to one side.
MRI scan findings:
Annular fissure – separation of the outer fibres of the vertebral disc (the annulus), usually a sign of disc degeneration.
Bony foraminal stenosis/narrowing – narrowing of the space between the vertebrae (located on each side) where the spinal nerves exit. This may be caused by disc herniation, degenerative disc disease, and spinal osteoarthritis.
Cord terminates at T12/L1 level – the location where the spinal cord actually ends (T12/L1 is normal).
Disc herniation – noted when any inner disc material (nucleus pulposis) extends beyond the normal limits of the disc (annular fibres). AKA disc bulge (for 50-100%), broad based herniation (25-50%), and focal herniation (<25%). (See picture below)
Distal cord and cauda equina – this is the end of the spinal cord, as it separates into different nerve bundles. [For interest, it is called ‘cauda equina’ as there are many nerve cords that join together to look a bit like horse hair!]
Focal nerve root impingement – pressure on the exiting nerve root, usually by a herniated disc. This pressure will interfere with the neural function, and along with pain may cause loss of function, weakness, sensation changes and temperature changes to the affected areas.
L5/S1 – the location indicator between the 5th Lumbar vertebrae (L5) and the top of the sacrum (S1). This can be used to describe the location of discs, facet joints. (The Lumbar spine is made up of 5 vertebrae: L1 to L5).
Loss of disc height/disc degenerative changes – reduction in the normal height of the disc. This is usually considered a normal part of ageing (as the discs dry out and become less flexible). (See picture below)
Osteophytes – bony growths that usually occur along the joint, or vertebral, margins. (AKA. Bone spurs). (See picture below)
Spondylitic changes (spondylosis) – degeneration of the joint(s) of the spine. Often used to describe osteoarthritic changes.
Spondylolisthesis – forward displacement of the upper vertebra over the lower vertebra.
Vertebral endplate changes – degeneration of the vertebral endplate, the upper/lower part of the vertebral body that connects with the discs.
In finishing…
Hopefully after reading this, you feel more comfortable reading the report from your scan and that it doesn’t seem so foreign. You will hopefully now know that a lumbar MRI with “Cord terminates at T12/L1 level. No central or foraminal stenosis noted. No spondylolisthesis, or spondylitic changes visible on scan” is just a fancy way to say that everything is normal!
On the other hand, if your scan mentions several of the above definitions, it would be wise to have a physiotherapist assess you. Hands-on treatment may be necessary initially, and a progression to a Clinical Pilates program may be the best option to prevent long-term pain. Your physiotherapist will discuss this with you during your appointment(s).
If you require any further information, or would like to make an appointment with one of our physiotherapists, please contact Therapia Physiotherapy and Pilates on 8221 5011. Please bring your scans with you to your appointment if you have them! Alternately, you can email us at info@therapia.com.au and we will respond as soon as possible.
References
“Degenerative Cervical Spine Disorders; Clear Explanations of Cervical Spine Conditions Causing Neck Pain”, Steven R. Garfin, Christopher M. Bono
Book Appointment