A Rounding Problem: Thoracic Kyphosis
What is it?
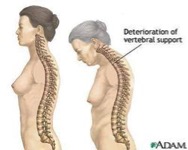
Also known as “Dowager’s Hump”, thoracic kyphosis is increased rounding of the upper back.
For some people, a thoracic kyphosis may start as a noticeable lump at the base of the neck, and may progress from there. The rounding of the spine causes increased pressure on the anterior (front) of the vertebrae, which can lead to vertebral degeneration and further rounding. It will also place the head in a forwards position, which may restrain neck movement and limit vision.
As a direct result, a thoracic kyphosis can cause middle back and neck pain, as well as lower back pain as a result of the forwards posture. When there is a significant kyphosis, it can also cause cardiorespiratory and digestive troubles, due to the reduced space in the chest cavity.
It is typically evident in women with osteoporosis, which causes degeneration and wearing of the vertebrae, and leads to rounding of the spine.
What are the causes?
- Posture, which is the most common type and is usually caused by ‘slouching’. The great news is that exercise, stretching and correcting your muscle imbalances can correct this cause!
- Degenerative diseases, such as Osteoporosis and Arthritis. These can lead to increased degeneration of the bone and vertebral discs, leading to increased rounding and weakness of the spine. Interestingly though, studies have strongly suggested that rather than osteoporosis being the cause of kyphosis, “postural forces are responsible for initiation of osteoporotic spinal deformity in elderly subjects” (1). This indicates that specific exercises and stretching will play an important role in preventing kyphosis from an early diagnosis of Osteoporosis.
- Developmental problems, such as Scheuermann’s Disease, a form of juvenile osteochondrosis of the spine.
- Congenital kyphosis, which occurs with incorrect development of an infant’s spinal column (in utero). Unfortunately surgery at an early age is the most helpful intervention for this cause, especially considering there are likely malformed, or fused, vertebrae.
- Injury, such as thoracic or rib fractures. These can go on to cause thoracic kyphosis, especially if left untreated, or treated poorly.
What can you do to help?
Posture
Ideally speaking, when sitting or standing, your posture should line up according to the “Plumb line”. This is an imaginary line, from your ear to the outer ankle, passing through the shoulder joint, outer hip, and outer knee. If these parts of your body are aligned, the spine will be in the most ideal position, and there will be no excessive forces placed on the spine.
1. Poor posture (Image TBA)
2. Improved posture (Image TBA)
Stretches
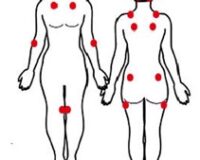
We know that there are some muscle groups that get tight with increased rounding of the spine, and most of them occur around the spine, shoulder blades, neck and front of the shoulders. As a result of tightening, these muscles can become so inflexible that they start to pull the spine into more kyphosis. The main muscle groups we are aiming to stretch include the upper back muscles, upper trapezius, levator scapulae, scalenes, anterior shoulder muscles, and pectorals.
Upper Trapezius/Levator Scapulae Stretch
Sit on hand
Tilt head to opposite side
Turn head to opposite shoulder
Hold for 10 seconds
Repeat every hour
Upper Back & Chest Stretch
Clasp hands behind you
Stretch them backwards, as far as comfortable
Hold 10 seconds, repeat every hour
Pectoral Stretch
Place forearms along the doorframe
Lean forwards (one leg forwards) & feel a stretch through the front of the chest
Hold 10 seconds
Repeat often
Cat Stretch/Child’s Pose
Start on all 4’s, then slowly sit backwards onto the feet
Stretch arms out forwards
Hold 10 seconds
Repeat often
Upper back strengthening exercises
These exercises are based on strengthening the muscles that we know weaken with thoracic kyphosis and with poor posture. The main muscle groups we are aiming to strengthen are those important muscles around the back and shoulder blades, including the back extensors, rhomboids, middle and lower trapezii. Clinical Pilates programs are also an excellent way to target specific weaknesses and improve posture and spinal health.
Prone Scapula Setting (with Arm Lift)
Lie on stomach, with small pillow under forehead
Keep hands on floor & pull shoulder blades down the back & in towards each other
Now lift the hands off the floor, while keeping the shoulder blades still
Lower hands, then lower shoulder blades
Perform 10 times
Half Press-Up
Lie on stomach, with hands under shoulders
Slowly press up with the hands and lift upper back, aiming to lift one vertebra at a time
Keep the stomach on the floor (don’t overextend the lower back)
Slowly lower back down, again one vertebra at a time
Perform 10 times
Thoracic Roller (with Arm Lift)
Lie lengthways along roller, knees bent up
Slowly lift arm up & over your head (aim to keep back flat)
Hold stretch for 10 seconds, slowly bring arms back
Repeat 3 times
Thoracic Extension with Roller
Start lying on stomach, hands over roller
Slowly lift head & upper back off floor, while rolling the roller towards you
Keep shoulders relaxed
Slowly lower back down
Repeat 10 times
As well as the above exercises, which can be performed safely and easily at home, there are some great exercises that require Pilates equipment, in particular the Reformer, Trapeze Table and Multi-Chair. For your interest, we have added a few more photos on the equipment below:
Back Extension (Multi-Chair)
IMAGE TBA
Prone Spine Extension (Trapeze Table)
IMAGE TBA
Cat Stretch (Trapeze Table)
IMAGE TBA
Chariots (Reformer)
IMAGE TBA
At Therapia Physiotherapy and Pilates, we are very aware of the problems caused by thoracic kyphosis, and we have an in-depth knowledge of techniques that will help to combat this issue. If you would like to book an appointment, or to talk to one of our physiotherapists about this, please contact us on (08) 8221 5011, or email us at info@therapia.com.au
Happy stretching!
References:
Keller TS, Harrison DE, Colloca CJ, Harrison DD, Janik TJ (2003). “Prediction of osteoporotic spinal deformity”.Spine 28 (5): 455–62
Book Appointment