Hip Bursitis
What is it?
Hip bursitis is a fairly common condition, and involves inflammation of the bursae around the hip joint. The bursa are small fluid-filled sacs, and are present to reduce the friction between tendons and the bone and ensure that everything is able to move smoothly. However they can become inflamed and painful with overuse, trauma and incorrect muscle use or weakness.
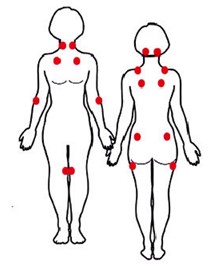
This picture demonstrates the bursae around the hip joint. There are many, however the bursitis we most commonly see is the Trochanteric Hip Bursitis. The trochanteric bursa cushions the outside of the hip against the gluteal muscles (especially gluteal maximus) and the Iliotibial Band (ITB). It is the most commonly injured as these are muscles very commonly used and therefore give the bursa a lot of work!
What are the causes?
As mentioned earlier, there are a few key causes of bursitis:
- Overuse (or muscles around the area) and repetitive stress – eg. With frequent running, jumping, squatting
- Trauma – e.g. a fall directly onto the outside of the hip (where there isn’t much padding)
- Incorrect muscle use and muscle patterns, causing altered biomechanics of the lower limb – this can also include weakness of the core muscles
- Weakness in the deeper gluteal muscles (Gluteus Medius and Minimus), and tightness in the Iliotibial Band (a band that runs down the outside of the thigh). As a result of the weakness in the deeper gluteal muscles, the gluteus maximus (biggest gluteal muscle) is forced to work more than it should, and so places more pressure in the bursa, which over time causes irritation and inflammation, and pain.
Interestingly, there are recent studies to suggest that hip bursitis does not often occur on its own, and that there is commonly some element of Gluteal pathology – especially tendinopathy of the Gluteus Medius (the main stabilising glute muscle). This may be the causative reason for weakness in this area, however it is not known yet as to which comes first – the bursitis, or the tendinopathy.
The picture below depicts the 3 gluteal muscles, and shows size and location (especially in relation to the outer hip area).
Picture courtesy of: http://www.nirschl.com/gluteus-medius-minimus-tendinosis-and-tears.asp
What are the signs and symptoms?
Commonly, sufferers will have a sharp pain on the side of their hip (worst directly over the bony outer part of the hip, and often tender to touch). This pain may extend down towards the knee, or even upwards towards the lower back. In fact, as the lower back, hip and knee are so closely linked, it is not uncommon to see problems in all areas along with hip bursitis, including pain, stiffness and restricted movement of these areas.
Sometimes there will also be a visible swelling over the outside of the hip, or even just the feeling of swelling.
There is often difficulty lying down on the side (due to the direct pressure), or even on the unaffected side (due to the stretch). This may cause trouble with sleeping.
Walking is also aggravating, especially first thing in the morning, or after a busy day. A limp may be present. There may also be pain with sitting cross-legged, or rising out of a chair after sitting for a while.
What are the treatment options?
There are several options when it comes to improving pain and keeping the bursitis away.
- Physiotherapy – this is highly successful for treating trochanteric bursitis. Initially, treatment will involve techniques to reduce the pain and swelling (eg. Ultrasound, ice, gentle massage, acupuncture, taping). Following this, your physiotherapist will aim to return full range of motion of the affected hip (and also lower back, knee if affected), correct any muscle imbalances around the hip and restore full function of the stabilising hip and core muscles, and work to eliminate any excess tightness that may be contributing to the problem. Due to the nature of trochanteric bursitis, and the danger of it recurring, a long-term program may be required. This may involve a Clinical Pilates program, or exercises you should continue afterwards (even if you aren’t feeling symptoms!)
- Ice – due to the inflammatory nature of trochanteric bursitis. Ice for 15 minutes at least once per day, and also after aggravating activities
- Anti-inflammatory medications
- Cortisone Injections – this involves injecting a corticosteroid (anti-inflammatory) along with a local anaesthetic into the bursa in order to settle the inflammation and stimulate healing. A guided injection (usually via ultrasound) is preferred as it will assist with needle placement. Cortisone injections can be very helpful, however repeat injections have been shown affect tendon health detrimentally – it would be wise to discuss side effects with your GP.
What can I do to help?
If sleeping is a problem, it can be improved in the short term with a pillow between the legs, to level out the hips when laying on the unaffected side.
Driving can be aided by sitting slightly higher (so your hips are not as bent). This may involve lifting the seat (in newer cars), or simply sitting on a pillow. Do make sure you can still reach the pedals & drive safely however!
There are several helpful exercises that will assist in recovery and strengthening. These will ideally be performed after the initial healing phase is completed (that is, when the pain and swelling have diminished). These exercises should be performed within your comfort levels, without causing pain.
Seated gluteal stretch
Sit on edge of chair, cross one foot over the other knee, SIT UP TALL, and lean forwards
There should be a comfortable stretch in the buttocks, or even down the side/back of the leg
Hold 20 seconds, repeat 3 times each leg
–
Lying gluteal stretch (Single knee to chest)
Lying on your back, slowly bring one knee up towards the opposite shoulder as far as comfortable.
You should feel a gentle, comfortable stretch in your lower back, or buttocks
Hold for 10 seconds, repeat 5 times
–
Bridging
Start on your back with knees bent (no pillow is best)
Slowly roll pelvis/hips off floor, followed by one vertebrae at a time
Aim to lower down, one vertebrae at a time
Try 10 repetitions
–
Prone Knee Bend
Start by lying on your tummy, feel the front of your hips on the floor.
Bend one knee to 90 degrees and then slowly lift thigh off floor (the front of your hips should stay firmly on the floor)
Once lifted, straighten your leg in the air, then slowly lower your straight leg
Repeat 10 times each leg
–
Clamshells
Start lying on your side with knees bent slightly. Make sure your shoulders, hips and feet are in a straight line.
Keep your feet together, back still and gently open your knees apart.
Repeat 10+ times on each leg, or until fatigue
* This exercise is especially helpful as it targets the Gluteus Medius
–
Advanced Clamshells
As above, make sure your body is aligned well.
This time, lift your feet up, keep your lower knee on the floor and lift your knees apart.
Repeat 10+ times on each leg, or until fatigue
In addition to these home exercises, your Physiotherapist may suggest a Clinical Pilates program – there are lots of helpful exercises on the Pilates equipment! This will be a program tailored to your specific needs, closely supervised and monitored.
If you have any queries about the above exercises, starting a Pilates program, or would like to talk with a Physiotherapist about your pain, please call us at Therapia Physiotherapy and Pilates on (08) 8221 5011, or email us at info@therapia.com.au
Book Appointment




