Plantar Fasciitis
An introduction to the biomechanics of the foot and the plantar fascia
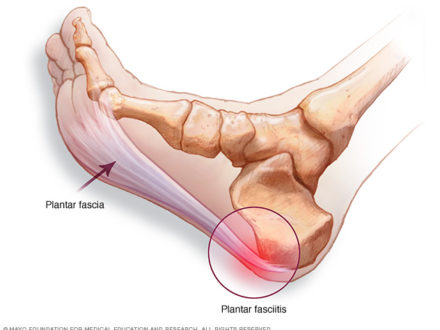
The plantar fascia originates on the calcaneus (heel bone). It then extends into five bands as it passes all 5 metatarsal heads and joins onto the toe bones (Moore, Dalley & Agur 2014). Please see in Figure 1.
Figure 1
The foot bones and its ligaments are in the formation of an arch-like triangular structure (Levangie & Norkin 2005) (Figure 2). The plantar fascia lines the bottom of the foot connecting the bones of the back and front of the foot to one another. It protects the muscles, blood vessels and neural structures that pass below it.
Figure 2
The foot is essential to our walking function. It enables push off from the ground, is very adaptable to changing surfaces, absorbs shock, and supports our entire body weight (Levangie & Norkin 2005).
There are many movements occurring in our feet and ankles that we are completely unaware of whilst walking. The ankle is capable of 6 movements: dorsiflexion, plantarflexion (Figure 3), inversion, eversion (Figure 4), abduction and adduction (Figure 5) (Levangie & Norkin 2005).
Figure 3
Figure 4
Figure 5
The combination of plantarflexion, inversion and adduction creates supination (commonly referred to as having a high arches) and the combination of dorsiflexion, eversion and abduction is referred to as pronation (also referred to as being flat footed) (Levangie & Norkin 2005) (Figure 6):
Figure 6
You can try this activity now, while sitting here reading this article, consciously try and rotate your knees outward, take note of the middle arch of your foot… Do you notice that your inner arch of your feet lifting higher? This is your feet supinating!
Then try and rotate your knees inwards so that they are facing one another. Notice how the inside of your feet falls closer to the floor? Your feet are supinating!
The walking cycle begins with the foot in a high arch position as the heel strikes the ground. The subtalar joint (the joint between the talus and heel bone seen in Figure 7), immediately pronates as it accepts the weight from the body (Levangie & Norkin 2005).
Figure 7
This flattening of the foot results in increased foot mobility for the absorption of ground reaction forces and adaption to uneven surfaces. The subtalar joint then starts to supinate the foot in preparation to allow the toe to come off of the ground. The high arch movement transforms the foot rigid and into a lever needed for propulsion (Levangie & Norkin 2005).
As we walk many forces stress the foot and could disrupt the maintenance of the arch. Vertical forces from body weight travel downward via the shinbone and tend to flatten the inner-sided arch (Levangie & Norkin 2005).
Ground reaction forces travel upward from the calcaneus and the metatarsal heads, which can further flatten the bones of the foot so that they are closer to the floor (Levangie & Norkin 2005).
The orientation of the plantar fascia helps maintain the arch throughout the walking cycle and contributes significantly to the appropriate amount and timing of how foot arch sits as we walk (Levangie & Norkin 2005).
During pronation, the talus slides forward. During supination, the talus moves backward into the ankle (Levangie & Norkin 2005).
Why does this matter?
This highlights the need for sufficient mobility through the joints in our ankle in order for the entire foot mechanics to work at its best function. It also suggests that if the joint is quite stiff and immobile, the arch position will be compromised and ultimately, the foot’s ability to maintain, or change the shape in arch throughout the movement, will be compromised.
Pronation (flat feet) increases the distance between the heel and toe bones and applies tension stress to the plantar fascia. Supination (high arched feet) also creates tension on the plantar fascia so that the foot can become a rigid lever arm, to propel the body forward (Levangie & Norkin 2005).
Inefficient foot function can lead to too much tension and consequently increased tissue stress. The foot must have a balance between pronation and supination. Too much or too little of either motion at the wrong time of the walking cycle potentially leads to dysfunction (Levangie & Norkin 2005).
What Causes Plantar Fascitis?
Plantar fascia pain results from excessive traction forces (increased tension) applied to the heel bone. This stretching can cause pain either to the plantar fascia itself or to the attachment to the bone (Tahririan et al. 2012). High tension could cause the growth of a spur that might be seen at the heel bone (Moore, Dalley & Agur 2014).
What symptoms are common to Plantar Fascitis?
- Heel pain especially with first steps in the morning
- Limited dorsiflexion (ability to lift toes upwards) and a tight achilles tendon (thick structure that passes the back of the heel)
- Limping or a preference to walk on your toes
- Pain is usually worse when you are barefoot, walking on hard surfaces or climbing stairs
- You suddenly increased your activity intensity just before this pain began (Moore, Dalley & Agur 2014)
What can the physiotherapists do to address and to treat it?
If plantar fasciitis results from increased plantar fascia tension, successful management depends on reversing the factors leading to excessive strain (Levangie & Norkin 2005).
Rehabilitation should focus on restoring muscle strength, improving muscle flexibility, and normalizing biomechanical influences. First, strengthening should incorporate all muscles involved with controlling pronation and facilitating the windlass mechanism (Bogla & Malone 2004) (the mechanism relating to the tensing of the plantar fascia to lift or lower the arch of the foot) (Levangie & Norkin 2005).
The rehabilitation plan should also use interventions designed to relieve any plantar fascia inflammation while correcting mechanical factors.
For example!!
Posterior Tibialis
The posterior tibialis muscle provides the most significant arch support during the single leg standing phase of the walking cycle. The posterior tibialis controls pronation (the flattening of the foot) and reduces the tension applied to the plantar fascia as the foot accepts the weight of the entire body (Levangie & Norkin 2005).
Excessive pronation (or flattening of the foot) can cause posterior tibialis weakness and therefore lengthening. The elongation minimizes efficient use of the foot’s arch because of instability during the push off phase during the walking cycle. Therefore it is clear, in many cases of plantar fasciitis, we must strengthen tibialis posterior (Levangie & Norkin 2005).
Plantar fasciitis in the rigid, higher-arched foot, results from the foot’s inability to even distribute force. Factors that contribute to under pronation include limited joint mobility, decreased plantar fascia extensibility, and increased muscle tightness (particularly in the Achilles – gastrocnemius and soleus).
This can be thought of as bowstring stretched very much so that the string is very tight.
Therefore treatment in this case should target increasing joint mobility, flexibility of the plantar fascia and the surrounding structures, and reducing the tightness of the muscle that are contributing.
Proximal muscle (muscle closer to the core) weakness, for example from the hip (gluteus medius, gluteus minimus, tensor fascia latae, or quadriceps muscles) can contribute to plantar fascia abnormalities (Rathleff et al. 2015).
Weakness in these muscles reduces their assistance in responding to any load applied through the lower limb, and results in greater transmission of force to the foot (Rathleff et al. 2015).
Furthermore, gluteus medius, gluteus minimus, and tensor fascia latae weakness can lead to anterior tiliting of the pelvis, affecting the position of the hip and knee joints, which in turn accelerate foot pronation (or flattening of the arch of the foot). Therefore, proximal muscle weaknesses can lead to poor shock absorption and decreased pronation control. (Rathleff et al. 2015). Figure 8 below shows the appropriate activation of muscles during the walking cycle, which is commonly altered due to different people having different musculature and walking patterns!
The excessive pronation of the foot this muscle weakness may place the joints further into a compromised posture, further reducing the need for the muscles to work and reducing their strength!
This can be seen in Figure 9 below:
Figure 9
The cause of weakness of the proximal muscles of the hip may also be contributed to by weak muscles of the core. This potentially due to insufficient mobility in neighbouring segments of the spine.
Did you realise, pain in your foot could be attributed to stiffness in our spine?? This is why it is vital to seek a professional opinion from a qualified physiotherapist. Please come and see us at Therapia Physiotherapy and Pilates, we would love to help out!
What Physiotherapy techniques do we offer to help?
It is important to remember each and every individual is different, and depending on the root cause of your presenting problem, the physiotherapists here at Therapia may use the following techniques to address and eventually reverse your presentation, provided they are suitable to your condition:
- Ultrasound (in acute stages)
- Muscle stretching and strengthening programs to address those contributing to poor foot and ankle alignment
- Mobilisation of tight structures contributing to the altered biomechanics of the lower limbs
- Dry Needling to promote healing, increase blood flow and wash away toxins
- Arch strengthening
- Taping to decrease the tensile forces placed on the plantar fascia
- Motor pattern retraining and rehabilitation
- Individualised Pilates program
- Strain-Counter-Strain techniques to reduce muscle tightness
- Footwear advice
We’re hoping the above information will be helpful for you. If you are concerned at all and if you would like to make an appointment with one of our physiotherapists, contact us at Therapia Physiotherapy and Pilates on (08) 8221 5011, or email us at info@therapia.com.au.
Book Appointment